
We know that change in general practice can be unsettling, especially when it impacts something as vital as the mental health care you provide to your community. Big changes are on the horizon with the Better Access initiative, and we’re here to help you walk through them with confidence and clarity.
From 1 November 2025, the familiar Medicare items for reviewing and continuing a patient’s Mental Health Treatment Plan (MHTP) are being removed from the MBS. These services will instead be billed using the standard time-tiered general consultation items you use every day. For many practices, particularly those with complex billing patterns, the financial implications could be significant. We’re here to break down exactly what’s happening and, most importantly, explore what it means for your practice’s sustainability.
First, let’s start with some reassuring news. The core of the Better Access initiative remains unchanged. Your patients will still be able to access up to 10 individual and 10 group sessions per calendar year. The item numbers used for the preparation of a new MHTP, such as 2715 and 2717, will also stay in place . These changes focus on the billing items used by GPs for reviews and ongoing care, not on the model of care itself.
Items being removed
The main items being removed form November 1st 2025 are the ones many practices use daily for MHTP reviews, specifically items 2712 and 2713. Alongside these, a range of other related mental health items are also being removed from the MBS, including items 277, 279, 92114, 92115, 92120, 92121, 92126, 92127, 92132, and 92133.
What does this look like from a billing perspective?
So, what does this look like in practice? Let’s look at one of the most common scenarios, a MHTP review. Previously, you would have billed an Item 2712. From 1 November, you will instead bill a standard time-tiered consult, like an Item 23 (for 6-19 minutes) or an Item 36 (for 20-39 minutes), based on the consult length. The item number billed will vary based on how much time you spend with the patient. Shorter reviews billed as an Item 23 will likely mean you are financially worse off than you were with the 2712. While, longer reviews that meet the criteria for an Item 36 will likely leave you in a better financial position. There is one significant piece of good news, the bulk billing incentives (BBI) will soon apply to all bulk-billed patients for these consults, not just concession card holders and children under 16, which simplifies things greatly.
Common billing scenarios (Pre November 2025)
| Items | Total fee value |
|---|---|
| 2712 | $83.65 |
| 2713 | $83.65 |
| 23 + 2712 | $127.55 |
| 965 + 2712 | $240.20 |
Items used in place of 2712 & 2713 from November 1 2025
| Item | Fee |
|---|---|
| 23 | $43.90 |
| 36 | $84.90 |
The biggest financial impact will come from the removal of co-billing. We know many practitioners have legitimately billed an MHTP review item, like a 2713, alongside a standard consult (like a 23 or 36) when addressing a separate, clinically distinct issue. From 1 November, this co-billing will no longer be possible. You will only be able to claim the single time-tiered attendance item, such as the 23 or 36, for the entire consultation. For many practices, this means a noticeable drop in billings for those specific encounters.
For example, a bulk-billed co-billing of 2713 + 36 in a metro (MM1) area for a non-concession eligible patient, previously totalled $168.55. Under the new structure, it would be billed as a single Item 36 co-billed with the relevant bulk billing incentive item, for a total fee of $106.75 in an MM1 practice. That’s a drop in billings of $61.80 for that one patient visit.
We understand this sounds confronting, however, for practices where MHTP reviews are commonly billed as a single item, there is the potential to grow billings under these new changes depending on the length of the consult and the items billed. Prior to November 2025, a single item 2712, bulk billed to a non-concession card holder would net a billing of $83.65. After November 1st 2025, this could be billed as an item 36 with an additional co-billed 10990 for a total fee of $106.75. Ultimately whether you will better or worse off under the new framework comes down to how mental health reviews have been billed historically, and what bulk billing incentives may apply within your MMM region.
To put it in perspective, Cubiko’s Touchstone benchmarking dataset shows that in 2025 so far, practices are on average providing roughly 44 Mental Health Treatment Plans per month, and 14 Mental Health Treatment Plan Reviews per month. These numbers are of course averages of practices across Australia, and you’re likely to find nuance within your own clinic depending on how much of an emphasis your practitioners place on mental health services.
At a volume of 14 reviews per month, we would not expect the financial impact of these changes to be significant to long term sustainability, regardless of whether your practice billings may be better or worse off under the new framework.
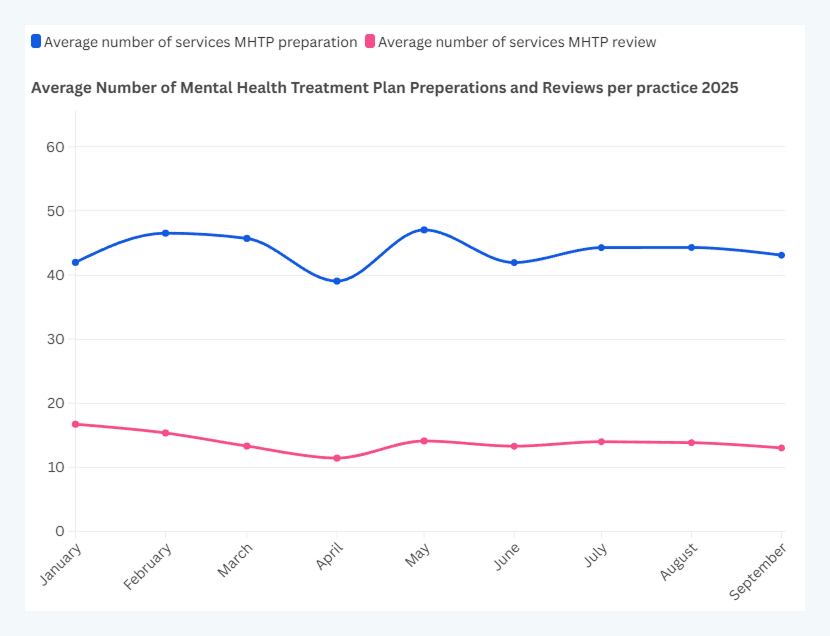
Cubiko Touchstone 2025, Average number of Mental Health Treatment Plan Preperations and Review per practice.
Silver linings
This is a chance to be proactive rather than reactive. This is a opportunity to embrace Continuous Quality Improvement (CQI) and re-evaluate your practice model. It’s time to analyse your workflows and billing practices, perhaps using PDSA (Plan-Do-Study-Act) cycles to find a new, sustainable path forward. Many practices may need to consider charging private or mixed fees for these longer, complex mental health consultations to maintain financial viability. This is also the perfect opportunity to ensure you are utilising the full MBS schedule to support your patients and your practice. This means proactively identifying patients who could benefit from Health Assessments, Chronic Disease Management plans, and team-based care. Embracing mental health case conferences, for example, allows for billable, holistic ‘wraparound care’ involving your nurses and the patient’s wider mental health team.
Perhaps the most important step is to bring your whole team on this journey. Be open and transparent with your patients about the changes. Many are often familiar with billing policies and will appreciate the clarity. Equip your reception and nursing teams with clear scripting and education so they feel confident and supported when explaining these new billing practices. By updating your fee schedules, empowering your team, and communicating with care, you can navigate this transition and continue to provide the vital mental health support your community depends on.


